1. American GDP vs. Open AI Energy Needs-Prof G Markets
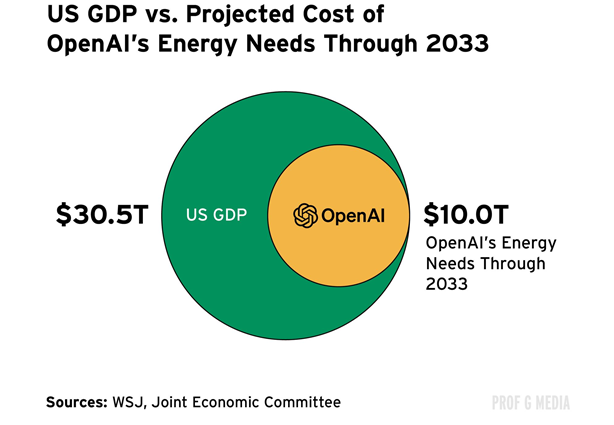
Prof G Market
2. Another Look at Breadth Improving Beyond Mag 7
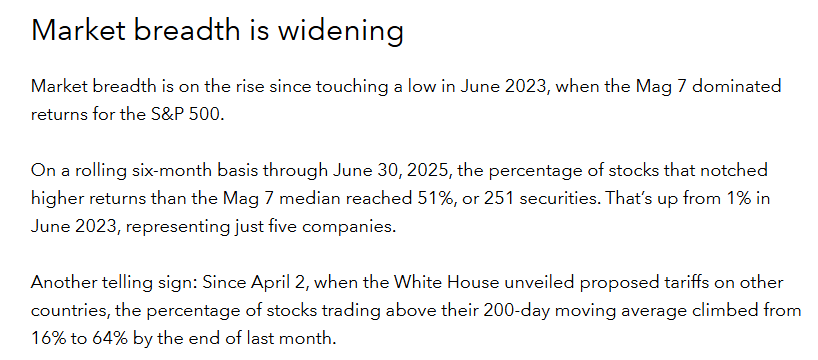
Capital Group
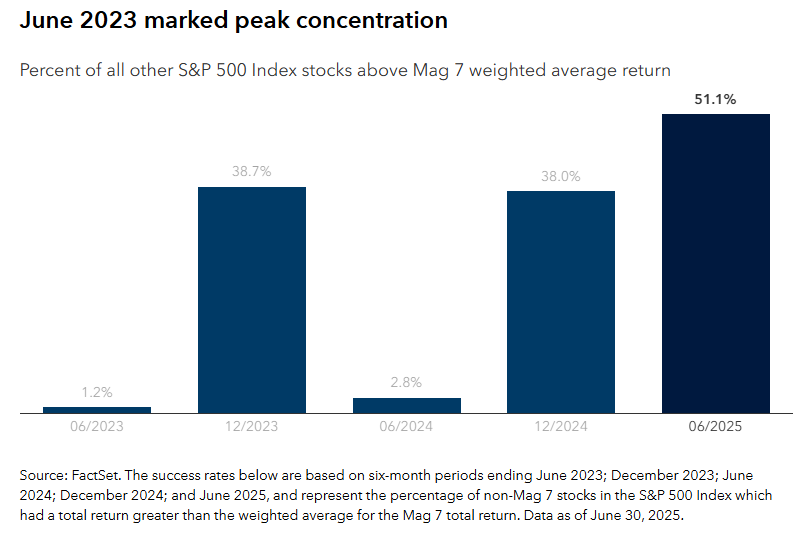
3. Semiconductor ETF Break-Out
StockCharts
4. Acceleration of Tech Adoption-Capital Group
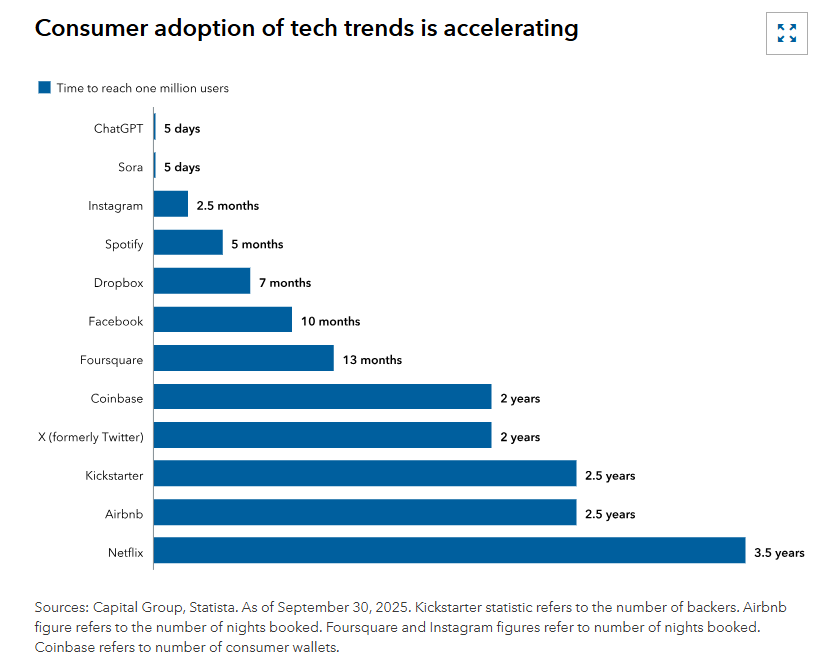
Capital Group
5. ChatGPT vs. Internet
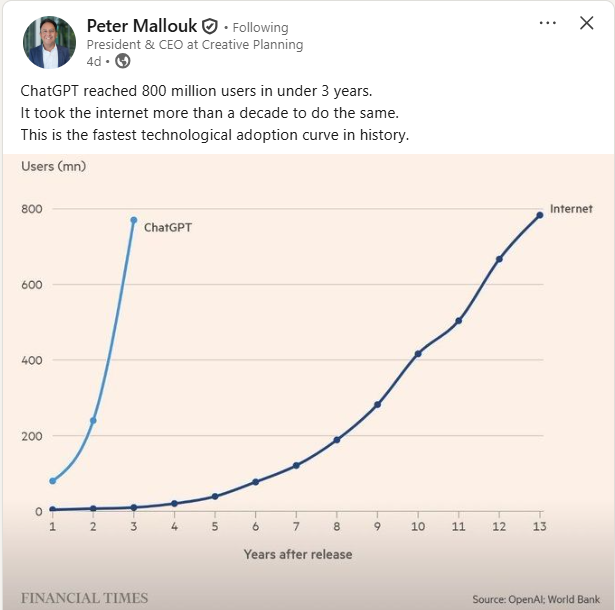
Peter Mallouk
6. 13M Meme Coins Launched in 2025
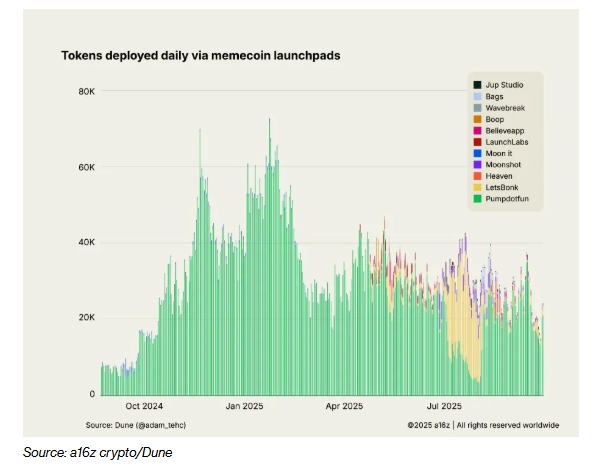
Bloomberg
7. Global Private Investment in AI …U.S. 10x China
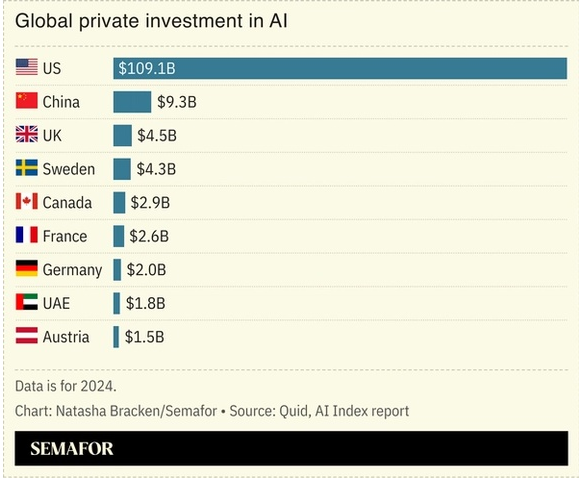
Semafor
8. Alternative Investments in 401k Plans….Evergreen Funds are Private Debt and Real Estate
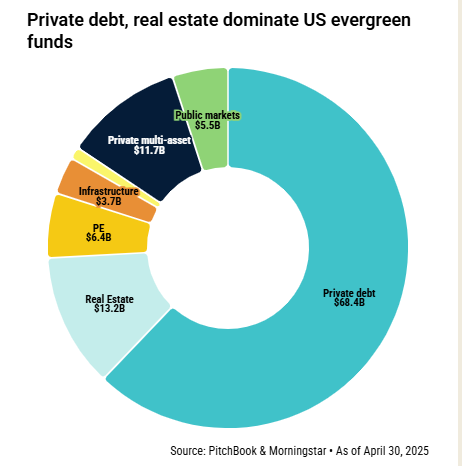
PitchBook
9. That was Fast…AI Equal Amount of Web Articles as Humans
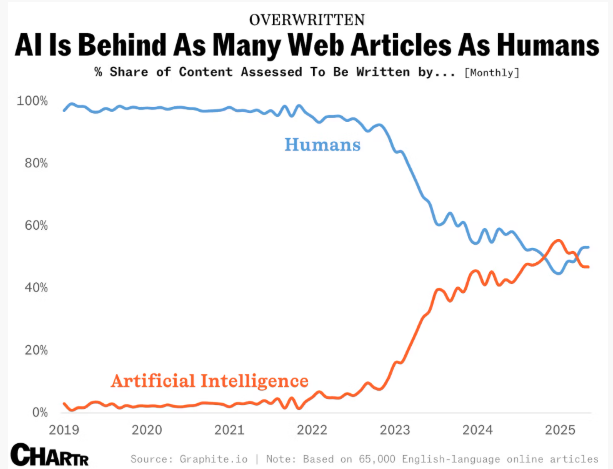
chartr
10. Guided missiles targeting tumor cells open a new route to combat cancer
A major European clinical research event in oncology gives a boost to antibody–drug conjugates, treatments that work like a Trojan horse, delivering chemotherapy to the interior of malignant cells
A researcher at the Clinic Barcelona Comprehensive Cancer Center handles biological samples in the lab. Jessica Mouzo
If more than half a century ago, science looked expectantly at the potential of chemotherapy to combat cancer; or 15 years ago, oncologists did the same with immunotherapy, which energized the immune system’s own defenses to attack tumor cells; now the spotlight has turned to an innovative treatment that is reaping promising results: antibody–drug conjugates (ADCs), treatments that function like a Trojan horse, delivering chemotherapy to the interior of tumor cells to destroy them. The European Society for Medical Oncology (ESMO) Congress, Europe’s main meeting for clinical cancer research, was held last week in Berlin, and it has given a boost to a new generation of these precision missiles. At the event, there were study presentations that demonstrated ADCs’ potential in several types of breast cancer and at various stages, not just metastatic.
These Trojan horses are formed by an antibody that targets a kind of antenna on the surface of tumor cells. These molecules carry a hidden chemotherapy payload, and when they reach their target, they bind to those receptors and release the entire drug into the tumor cells to selectively kill them. “ADCs are here to stay. It’s a validated line of research and it is like a highway along which we can continue to advance,” noted Aleix Prat, director of the Clinic Barcelona Comprehensive Cancer Center. Other studies presented at the event showed that this therapeutic approach also has potential for other tumors, such as ovarian, endometrial, and pancreatic cancers.
In breast cancer, these precision missiles have shaken up the prognosis of the most aggressive tumors. They entered the therapeutic arsenal more than a decade ago, but new generations of these drugs are gaining more ground. Three years ago, for example, research demonstrated that one of the new ADCs, trastuzumab-deruxtecan, increased the survival rate of women with HER2+ tumors (this subgroup accounts for 20% of all breast cancers) in metastatic stages. And a new study presented this year at ESMO and published simultaneously in the prestigious New England Journal of Medicine (NEJM) has also shown that another of these new precision missiles, sacituzumab govitecan, is more effective than conventional chemotherapy in treating triple-negative breast cancer (the most aggressive type, affecting 15% of patients) in advanced stages: median progression-free survival was almost 10 months in those treated with this Trojan horse (in those treated with chemotherapy alone it was seven months).
Javier Cortés, director of the International Breast Cancer Center in Barcelona and author of this research, asserts that, with this study, science confirms that when breast cancer metastasis appear; that is, when malignant cells have spread to other parts of the body, these drugs are positioned as the first treatment option. “This study adds another twist and improves the prognosis for these patients. Little by little, we are making slow but steady progress. At this congress, immunoconjugates have positioned themselves as the most innovative, the hottest, and the most spectacular,” notes the doctor, who is also scientific director of the IOB Institute of Oncology Madrid.
But this therapeutic strategy isn’t just suitable for the most advanced stages of cancer. Another study presented at the conference and published in the Annals of Oncology showed that in patients with high-risk, HER2-positive early breast cancer — who are more likely to have the disease recur — administering the ADC trastuzumab-deruxtecan followed by standard therapy before surgery improves the pathological complete response. This means that there are no tumor cells in the breast or lymph nodes at the time of surgery after this treatment, a key parameter for reducing the risk of relapse.
Santiago Escrivá de Romaní, an oncologist at the Breast Cancer Group at the Vall d’Hebron Institute of Oncology, participated in this research: “We found an 11% higher rate of complete pathological response [when incorporating ADCs into treatment].” The doctor asserts that the development of Trojan horses is “a turning point” in oncology: “ADCs are gaining significant traction. They don’t allow us to rule out chemotherapy, but they greatly help us target it more precisely to tumor cells,” he adds.
Regarding this research, Prat asserts that in these early contexts, the therapeutic potential they anticipate from these Trojan horses means that “they can cure more patients.”